Best
Clinical Data Integration
Products
Clinical Data Integration refers to the process of combining and harmonizing data from various sources within healthcare systems to create a unified and comprehensive view of patient information. It involves integrating data from electronic health records (EHRs), clinical systems, laboratory systems, imaging systems, and other relevant sources to facilitate better patient care, clinical research, and healthcare management. Read more
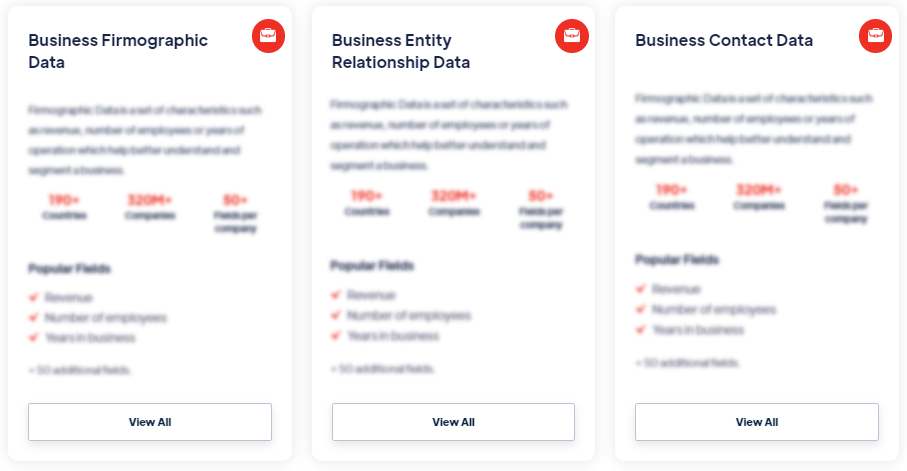
Our Data Integrations


Request Data Sample for
Clinical Data Integration

Browse the Data Marketplace
Frequently Asked Questions
What is Clinical Data Integration?
Clinical Data Integration refers to the process of combining
and harmonizing data from various sources within healthcare
systems to create a unified and comprehensive view of patient
information. It involves integrating data from electronic health
records (EHRs), clinical systems, laboratory systems, imaging
systems, and other relevant sources to facilitate better patient
care, clinical research, and healthcare management.
What are the key challenges in Clinical Data Integration?
Clinical Data Integration faces several challenges that need to
be addressed for successful implementation. One challenge is the
lack of standardized data formats and terminologies across
different systems. Variations in data structures, coding
systems, and terminology standards make it difficult to merge
and analyze data seamlessly. Efforts to standardize data formats
and adopt common terminologies, such as SNOMED CT or LOINC, can
help address this challenge. Another challenge is the
heterogeneity of data sources, each with its own data models,
schemas, and data quality issues. Data transformation and
mapping are required to align and reconcile data from different
sources, ensuring consistency and accuracy. Interoperability
challenges also arise due to the diversity of clinical systems,
interfaces, and data exchange protocols. Implementing
interoperability standards, such as HL7 FHIR or DICOM,
facilitates smooth data integration and exchange between
systems. Privacy and security concerns related to patient data
must also be addressed during the integration process, ensuring
compliance with relevant regulations and protecting patient
privacy.
What are the benefits of Clinical Data Integration?
Clinical Data Integration offers several benefits in healthcare
delivery, research, and decision-making. It enables a holistic
view of patient information by consolidating data from multiple
sources, improving care coordination and patient outcomes.
Integrated data can facilitate clinical decision support
systems, helping healthcare providers make informed decisions
based on comprehensive patient information. It supports
population health management by providing insights into disease
prevalence, treatment outcomes, and resource utilization
patterns. Clinical Data Integration enhances clinical research
capabilities by enabling access to large and diverse datasets,
enabling researchers to conduct studies and generate evidence
more effectively. It also facilitates secondary use of data for
epidemiological studies, quality improvement initiatives, and
public health surveillance.
What are the key considerations in Clinical Data
Integration?
Several considerations should be taken into account during
Clinical Data Integration. Data governance is crucial to ensure
data quality, security, and compliance with regulatory
requirements. Establishing data standards, data ownership
policies, and data access controls are essential components of
data governance. Interoperability standards and data exchange
protocols should be implemented to enable seamless integration
and exchange of data between systems. Integration should focus
on meaningful and relevant data elements, prioritizing the data
needed for specific use cases. Data mapping and transformation
techniques should be employed to align and reconcile data from
different sources. Data validation and quality assurance
processes are important to identify and address data
inconsistencies, errors, or outliers. Ongoing monitoring and
maintenance of the integrated data are necessary to ensure its
accuracy and integrity over time.
What technologies or tools are commonly used in Clinical Data
Integration?
Various technologies and tools are used in Clinical Data
Integration. Integration engines or middleware solutions, such
as Mirth Connect or InterSystems Ensemble, facilitate data
exchange and integration between different systems. Data
integration platforms, such as Informatica or Talend, provide
capabilities for data transformation, mapping, and
harmonization. Application Programming Interfaces (APIs) and web
services enable secure and standardized data exchange between
systems. Healthcare interoperability standards, such as HL7,
DICOM, or FHIR, play a significant role in enabling data
integration. Master Data Management (MDM) systems help manage
and synchronize patient identifiers and other reference data
across systems. Data warehouse and data repository solutions,
such as Oracle or Microsoft SQL Server, are often utilized to
store and consolidate integrated data.
What are the challenges in ensuring data quality in Clinical
Data Integration?
Ensuring data quality in Clinical Data Integration can be
challenging due to various factors. Data inconsistencies,
errors, and missing values may exist in the source systems,
requiring data cleaning and transformation efforts. Data mapping
and harmonization across different data models and terminologies
can introduce complexities and potential inaccuracies. Data
validation processes need to be implemented to identify and
rectify data quality issues, including outliers, duplicates, or
invalid values. Ongoing data quality monitoring and maintenance
are necessary to ensure the integrity and accuracy of the
integrated data. Collaborative efforts between data stewards,
data custodians, and healthcare providers are important to
establish data quality standards, define data quality metrics,
and implement data validation processes throughout the
integration lifecycle.