Best
Electronic health records (EHR) data
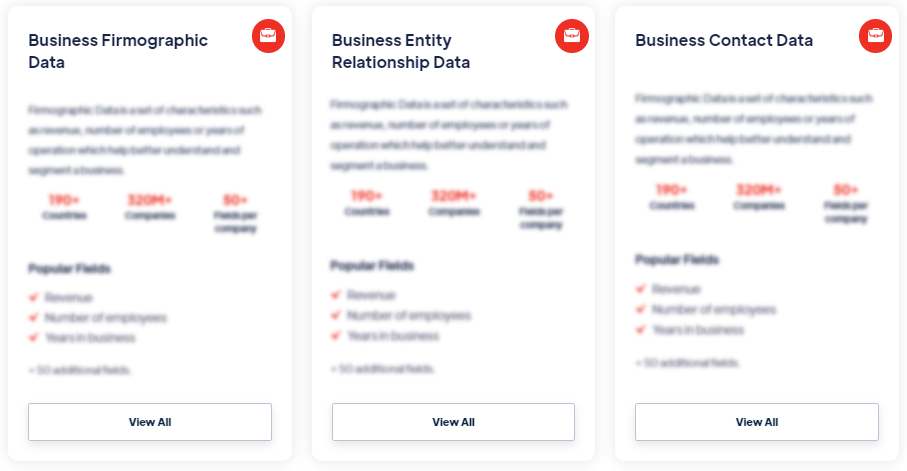
Products
Electronic Health Record (EHR) Data refers to digital and computerized versions of patients' health records. It includes comprehensive and longitudinal information about a patient's medical history, diagnoses, treatments, medications, lab results, immunizations, allergies, and other relevant healthcare data. EHR data is typically stored and managed in electronic health record systems, allowing healthcare providers to access and share patient information securely. Read more
Our Data Integrations


Request Data Sample for
Electronic health records (EHR) data

Browse the Data Marketplace
Frequently Asked Questions
1. What is Electronic Health Record (EHR) Data?
Electronic Health Record (EHR) Data refers to digital and
computerized versions of patients' health records. It
includes comprehensive and longitudinal information about a
patient's medical history, diagnoses, treatments,
medications, lab results, immunizations, allergies, and other
relevant healthcare data. EHR data is typically stored and
managed in electronic health record systems, allowing healthcare
providers to access and share patient information securely.
2. What types of information are included in Electronic
Health Record (EHR) Data?
Electronic Health Record (EHR) Data encompasses various types
of patient information. It includes demographic data (e.g.,
name, age, gender, contact information), medical history (e.g.,
past illnesses, surgeries, hospitalizations), current and past
medications, allergy information, immunization records,
laboratory and diagnostic test results, clinical notes, progress
notes, discharge summaries, and physician orders. It may also
include vital signs, medical images, family medical history,
social history, and patient-reported data such as symptoms, pain
levels, and lifestyle information.
3. How is Electronic Health Record (EHR) Data collected?
Electronic Health Record (EHR) Data is collected from various
sources in healthcare settings. Healthcare providers input
patient information directly into the electronic health record
system during consultations, examinations, and treatments.
Medical devices and equipment can capture and integrate data
directly into the EHR system, such as vital signs monitors,
laboratory equipment, and imaging systems. Electronic
prescriptions and pharmacy systems also contribute to
medication-related data in EHRs. Additionally, patients
themselves may provide data through online portals, personal
health apps, or self-reporting tools, allowing them to actively
participate in their care and contribute to their EHR data.
4. How is Electronic Health Record (EHR) Data used?
Electronic Health Record (EHR) Data serves multiple purposes in
healthcare. It enables healthcare providers to have a
comprehensive view of a patient's medical history,
facilitating accurate diagnosis, treatment planning, and
monitoring of patient progress. EHR data supports clinical
decision-making, ensuring that healthcare professionals have
access to up-to-date and relevant patient information. It also
aids in care coordination among different healthcare providers
and settings, allowing for seamless information exchange. EHR
data is utilized for population health management, quality
improvement initiatives, medical research, and reporting
purposes to monitor healthcare outcomes, trends, and adherence
to regulatory standards.
5. What are the challenges in working with Electronic Health
Record (EHR) Data?
Working with Electronic Health Record (EHR) Data presents
several challenges. Data interoperability and standardization
can be a barrier due to the use of different EHR systems and
data formats across healthcare organizations. Ensuring data
privacy and security is critical to protect patient
confidentiality and comply with healthcare regulations, such as
the Health Insurance Portability and Accountability Act (HIPAA).
Data quality and completeness issues may arise due to
documentation variations, human errors, or inconsistent data
entry practices. Managing and analyzing large volumes of EHR
data can also pose technical and computational challenges,
requiring robust infrastructure and analytical capabilities.
6. What are the benefits of using Electronic Health Record
(EHR) Data?
Using Electronic Health Record (EHR) Data offers several
benefits in healthcare delivery and management. It promotes
efficient and accurate patient care by providing healthcare
providers with comprehensive and real-time patient information.
EHR data supports clinical decision support systems, alerting
healthcare professionals to potential drug interactions,
allergies, or abnormal test results. It enhances care
coordination and patient safety through secure information
sharing among healthcare providers. EHR data contributes to
medical research, clinical trials, and public health
initiatives, allowing for population-level analysis and
evidence-based decision-making. It also enables patients to
access and manage their health information, empowering them to
be active participants in their healthcare journey.
7. What are the best practices for using Electronic Health
Record (EHR) Data?
To effectively use Electronic Health Record (EHR) Data, several
best practices should be followed. Ensuring data privacy and
security through strong access controls, encryption, and audit
trails is essential to protect patient information. Promoting
data interoperability and standardization efforts can facilitate
seamless information exchange and continuity of care across
different healthcare settings. Implementing data governance and
data quality management processes can help address data
integrity issues and ensure the accuracy and completeness of EHR
data. Engaging patients and obtaining their informed consent for
data sharing and research purposes is crucial to uphold ethical
standards. Collaboration and partnerships among healthcare
organizations, technology vendors, researchers, and regulatory
bodies are vital to drive innovation, address challenges, and
advance the use of EHR data in improving healthcare outcomes.