Best
Patient Electronic Health Records Data
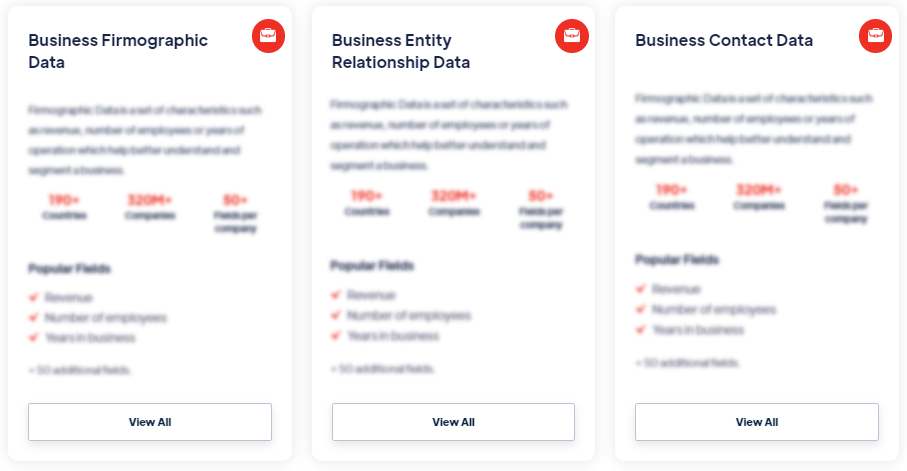
Products
Patient Electronic Health Records (EHRs) data refers to digital records that contain comprehensive information about an individual's medical history, diagnoses, treatments, medications, allergies, laboratory results, imaging reports, and other relevant healthcare data. EHRs are electronic versions of traditional paper-based medical records and are stored and accessed through secure health information systems. Read more
Our Data Integrations


Request Data Sample for
Patient Electronic Health Records Data

Browse the Data Marketplace
Frequently Asked Questions
1. What are Patient Electronic Health Records (EHRs) Data?
Patient Electronic Health Records (EHRs) data refers to digital
records that contain comprehensive information about an
individual's medical history, diagnoses, treatments,
medications, allergies, laboratory results, imaging reports, and
other relevant healthcare data. EHRs are electronic versions of
traditional paper-based medical records and are stored and
accessed through secure health information systems.
2. How is Patient EHRs Data collected?
Patient EHRs data is collected from various sources, including
healthcare providers, hospitals, clinics, laboratories, and
pharmacies. It is entered into electronic systems by healthcare
professionals during patient encounters, such as doctor visits,
hospital admissions, laboratory tests, and medication
prescriptions. Patient EHRs data can also be gathered from other
health-related sources, such as wearable devices and
patient-reported outcomes.
3. What are the benefits of Patient EHRs Data?
Patient EHRs data provides healthcare providers with a
comprehensive and centralized view of a patient's medical
history, facilitating improved care coordination, clinical
decision-making, and patient safety. EHRs enable efficient
access to patient information, reduce medical errors, enhance
communication between healthcare providers, and support
continuity of care. They also enable patients to access their
own health information, participate in their care, and engage in
shared decision-making.
4. How is Patient EHRs Data managed and protected?
Patient EHRs data is managed through secure health information
systems that adhere to strict privacy and security regulations,
such as HIPAA in the United States. Access to patient EHRs is
typically restricted to authorized healthcare professionals and
is protected by user authentication, data encryption, and audit
trails. Data backup and disaster recovery measures are in place
to ensure the integrity and availability of the data.
5. What are the challenges in working with Patient EHRs
Data?
Working with patient EHRs data poses challenges related to data
interoperability, standardization, and data quality. Ensuring
accurate and complete data entry, maintaining data consistency
across different healthcare settings, and integrating data from
disparate systems can be complex. Protecting patient privacy and
ensuring data security are ongoing challenges in managing and
sharing EHRs data.
6. How is Patient EHRs Data used for research and
analytics?
Patient EHRs data is valuable for medical research,
epidemiological studies, health outcomes analysis, and
healthcare analytics. Aggregated and anonymized EHRs data can
provide insights into disease patterns, treatment effectiveness,
medication safety, and population health trends. Researchers and
data analysts can leverage EHRs data to identify patterns,
conduct clinical studies, develop predictive models, and inform
evidence-based healthcare practices.
7. What are the ethical considerations in using Patient EHRs
Data?
Ethical considerations in using patient EHRs data include
ensuring patient privacy and confidentiality, obtaining informed
consent for research purposes, de-identifying or anonymizing
data to protect patient identities, and adhering to ethical
guidelines and regulations. Balancing the benefits of using EHRs
data for research and public health purposes with the protection
of patient rights and privacy is of utmost importance.
â€